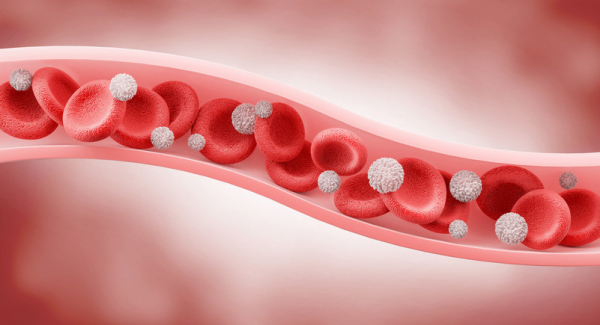
Blood circulation is vital to our health. Our arteries deliver oxygen, energy-rich nutrients, hormones, immune cells, and other essentials throughout the body. When deliveries are cut off, organs and tissue can be irreversibly damaged within minutes.
But a second part of blood circulation is also vitally important: the return trip. After our arteries deliver the goods, our blood must return to the lungs to pick up more oxygen, stock up on nutrients, get rid of carbon dioxide, and head back to the heart to be pumped out again. In this way, blood is in continuous motion, ensuring organs and tissues get what they need while waste products are removed.
The vessels designed for the return trip are your veins. Read on for answers to questions about how veins work, what can interfere with their ability to work smoothly, and five ways to keep thousands of miles of these blood vessels healthy.
What are veins and what do they do?
Perhaps you haven't thought much about your veins. Or if you have, maybe you focused on varicose veins, those swollen, unsightly purplish vessels that may be visible just beneath the skin of the legs. Or perhaps you had a blood test and the person taking the blood had a hard time finding a "good vein." But these are just a small part of vein world.
Veins make up a network of connecting tubes throughout the human body, ranging in size from 1 mm (about the size of a pencil point) to 2 cm (about the size of a quarter), that bring blood low in oxygen back to the lungs to reload with oxygen. Then four pulmonary veins carry oxygen-rich blood from the lungs to the heart. (Fun fact: some people have three or five pulmonary veins, but most of us have four.)
Often, major veins are found alongside similarly named arteries, like a highway with cars moving in opposite directions: in the upper arm, for example, the axillary vein lies next to the axillary artery; in the kidney, the renal vein runs alongside the renal artery.
How do veins help keep blood flowing?
Let's start by picturing tiny red blood cells loaded up with oxygen. Now imagine you're a red blood cell that has just traveled from the heart through the arteries to a calf muscle of someone who is jogging. After you drop off the much-needed oxygen and pick up waste products like carbon dioxide, you need to get back to the heart — fast! — because exercising muscles need extra oxygen.
But wait. As you head back to the lungs to load up on more oxygen and release carbon dioxide, there's a steep climb straight up. How can you make it back to the lungs without help?
Fortunately, veins have tiny valves within them that allow blood to flow in only one direction. When muscles contract near larger veins, they pump blood toward the lungs. In addition, taking in a breath creates a sort of suction that pulls blood toward the lungs. Without these forces encouraging blood to flow in the right direction through the veins, blood flowing into the legs would pool there, causing dangerously high pressure and swelling.
Why are veins blue?
Actually, they aren't. People think they're blue because that's often how they appear in diagrams and illustrations. But that's just to set them apart from the bright red arteries.
The veins on the back of your hand may appear blue if you have light-colored skin. That's an illusion due to the way light is absorbed by the skin. In people with darker skin tones, veins tend to blend in more.
If you could look at veins directly, without any skin in the way, they'd appear pale because they are naturally colorless, or dark red due to the blood inside them.
What sort of problems can occur in veins?
Blood clots, varicose veins, and venous insufficiency are some of the most common health conditions affecting the veins:
- Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, blocking blood flow. This condition is potentially serious because clots in deep veins can travel to the lungs, causing a life-threatening pulmonary embolism by blocking an artery that delivers blood to part of the lungs.
- Superficial thrombophlebitis is a blood clot in a small vein just under the skin. This causes inflammation and pain.
- Varicose veins are small veins under the skin that swell and twist. While these may be harmless, they can cause pain and are occasionally complicated by blood clots.
- Venous insufficiency occurs when the valves in veins are damaged — due to aging or prior blood clots, for example. The blood flow through the veins may be impaired, leading to leg swelling, increased pressure, inflamed skin, and poor healing.
One far more rare condition goes by the impressive name of phlegmasia cerulea dolens. It is a serious complication of DVT in which the obstruction of blood flow through a deep vein leads to blocked blood flow through nearby arteries. That can cause gangrene and the need for amputation.
All of these conditions can affect circulation temporarily or in a lasting way. Treatments are aimed at restoring circulation, if possible.
Top 5 ways to improve vein health
Healthy veins help the heart, brain, and every other part of your body. Here are five ways to improve vein health, even if you already have vein disease:
- Be active. Exercise regularly and avoid prolonged standing or sitting.
- Choose healthy foods, such as those in a plant-based, heart-healthy diet.
- Maintain a healthy weight.
- Don't smoke.
- Wear compression stockings if you already have vein disease such as venous insufficiency.
And of course, seek medical care for unexplained swelling, inflammation, or ulcers on your legs, ankles, or feet.
The bottom line
Our veins are busy around the clock, shuttling blood from distant sites back to the lungs and heart, which pumps enriched blood out again. Without veins, blood circulation could not happen. They're a good example of how many parts of your amazing body are easy to overlook until something goes wrong.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD